Clothing
- Make sure the tube or button extension set is securely attached to your child to avoid tension.
- Avoid clothing with a tight belt so that it does not rub against the stoma or get caught in the tube or button.
- Ideally, wear clothing that covers the button or enterostomy long tube (eg, long t-shirt, one-piece pyjamas, button-down sleepsuit, overalls).
Bathing and swimming
Bathing:
- Your child can take a bath or shower with his or her feeding tube or button, unless your healthcare team advises otherwise. Make sure the cover is securely in place.
- You can take advantage of the bath time to change the nasogastric tube; make sure the skin on the cheek is dry before reinserting the tube after the bath, if necessary.
Ostomy care:
- Clean the skin around the stoma with a small washcloth soaked in room temperature tap water and unscented mild soap (eg, “Dove”). Start on the inside (the area of skin closest to the stoma) and clean outward (the area of skin furthest from the stoma).
- Gently lift the button or the long tube external bolster and clean the ostomy site in the same manner.
- Observe the skin around the stoma; it should be clean, dry, and intact (same appearance as usual: similar to the color of the belly or slightly pinkish). Check for signs of infection (redness, tenderness, swelling, discharge different from the usual yellowish or brownish discharge, bad odour).
- It is normal for a small amount of yellowish or brownish discharge to come out of the stoma. They may become crusty as they dry. You can easily remove them with a cotton swab. Rinse and dry the skin well.
- If your child has had a stoma for less than 6-8 weeks (or other length of time, as recommended by your healthcare team), check with your healthcare team to see if cleaning the stoma site with saline solution is needed. Refer to your healthcare team for the recipe and storage of homemade saline solution, if recommended.
- As with all children, avoid bubble baths and scented oils.
- Do not apply cream or lotion to the skin around the stoma unless recommended by your healthcare team.
- If there is a small amount of milk or nutritional formula leakage, you can place a compress under the button or around the tube on the skin to absorb the leakage and protect the skin; change the compress as soon as it is wet to keep the skin clean and dry. You can purchase button pads, made for children, from many online retailers (eg, www.feedingtubeawareness.org/g-gj-tube-pads/). Discuss this with your healthcare team.
Mouth care:
- Even if your child is not eating, your child’s mouth should be cleaned at least twice a day.
- If your child has no teeth, use a small face cloth or a compress dampened with water and rolled around your index finger, to gently rub your child’s gums and tongue.
- Once teeth start to appear, brush your child’s teeth after each meal and at bedtime. Since young children have a tendency to swallow toothpaste instead of spitting it out, use only the size of a small grain of rice in children under 2 years old and the size of a small pea in children up to 6 years old. Use this time to also gently massage their gums with the toothbrush.
- As your child matures, teach and supervise brushing of the teeth.
- Apply, if required, a hydrating lip balm.
Nasal hygiene:
- In all children, secretions, along with bacteria and viruses collect in the nose. Keeping your child’s nose clean helps prevent lung infections.
- If your child cannot blow his/her nose effectively, refer to your healthcare team for the appropriate technique for nasal hygiene with a saline solution that will allow your child to clear his/her nose properly (recipe and storage of the “homemade” saline solution, quantity to use, how to proceed according to your child’s age, etc.). To this end, you can refer to the brochure published by the Centre hospitalier universitaire Ste-Justine that explains the technique of nasal hygiene: Nasal hygiene.
Swimming:
- Immediately following tube placement, your child can bathe according to the recommendations of the healthcare team.
- Unplug your child from the feeding system and remove the extension set, if in place, before swimming.
- Make sure the tube is securely fastened so that it will not get snagged or ripped off while swimming.
- Make sure the cover on the nasal tube, button feeding port or enterostomy long tube ports is securely closed.
- Consult your healthcare team for recommendations specific to your child.
Sleeping
- As with all children under one year of age, lay your baby on his or her back to sleep.
- If applicable, refer to your healthcare team to obtain an IV pole for overnight feedings.
Nutrition and hydration
- Your healthcare team is responsible for identifying the specific type of nutritional formula for your child. Follow their instructions for preparation, if applicable, and for the amount to give according to the feeding schedule agreed upon with you.
- Always check the expiry date on the original container or package before preparing or using the product; do not use products that are past their expiry date.
For ease of reading the rest of the text, the word (nutritional) “formula” also includes “breast milk”, “fortified breast milk” or “infant formula”.
- Preparation of the nutritional formula:
- Follow the manufacturer’s or your healthcare team’s instructions carefully.
- Confirm with your healthcare team the type of water, if any, to be used for preparation: tap water, sterile water or cooled boiled water. The type of water varies according to the age and condition of your child.
- Conservation of the nutritional formula:
- Follow the manufacturer’s or your healthcare team’s instructions carefully.
- The conservation time of the formula depends on how it is prepared (ready-to-use or reconstituted from liquid concentrate or powder).
- Unopened original containers or packaging may be stored until their expiry date.
- Remaining portions should be stored in a clean, airtight container.
- Administer the formula at the temperature your child can tolerate, as recommended by your healthcare team.
- Do not reheat the container in the microwave.
- The length of time the formula is kept in the feeding bag varies according to several factors (eg, the form of the product used, whether or not supplements have been added, etc.). Follow the instructions of the manufacturer or your healthcare team. Pour only the amount needed for the feeding session and discard the formula that remains in the bag afterwards.
The following are general recommendations for the preparation and storage of the nutritional formula:
Preparation and conservation of the nutritional formula
| Formats | Preparation | Conservation: Remaining portion of the prepared formula | Conservation: Remaining portion of the original container |
| Ready to serve |
|
X |
|
| Liquid concentrate |
|
|
|
| Powder |
|
|
|

- Precautions for the content of the feeding bag:
- Check that the feeding bag and tubing have been rinsed thoroughly before use.
- Do not add new formula to the bag if there is any left over from the previous feeding session.
- Check with your healthcare team as to how much formula to put in the feeding bag to ensure that it will keep for the correct conservation time.
- Always check that the formula is at the temperature your child can tolerate, as recommended by your healthcare team, before transferring it to the feeding bag.
- Never place the filled feeding bag near a source of heat (eg, a furnace) or in a sunny place.
- Follow the recommended conservation time for the formula in the feeding bag to avoid contamination and the development of an infection in your child.
- Your healthcare team may recommend pureed (blenderized) tube or button feeding for your child. If this is the case, they will give you the appropriate details.
- Discuss with your healthcare team whether your child’s condition also allows for drinking and/or eating by mouth.
- Even if your child is receiving enteral feeding, you can encourage your child to sit at the table while other family members eat their meal. It is important that your child participates in the meals at the table. Mealtime is a social activity for the whole family. If your child can eat by mouth, take advantage of these opportunities to encourage your child to touch and taste the food.
- You can hold your baby in your arms during feeding sessions as if you were feeding by breast or bottle.
- Discuss with your healthcare team the best position for your child during feeding to help ease digestion, avoid discomfort (eg, nausea, vomiting, reflux) and the risk of aspiration (accidental entry of formula into the lungs).
- You can burp your baby after feeding.
- If your child has a stoma, you can also decompress (or vent) the stomach prior to feeds, as taught by your healthcare team; this will help release gas and relieve bloating.
Activities
- Your child can continue regular daily activities, according to the limits of your child’s health conditions. Make sure that the button or enterostomy long tube is always well protected. Discuss this with your healthcare team.
- However, your child should avoid:
- activities that may cause the tube or button to move accidentally (eg, pulling, contact sports),
- the use of scissors near the tube and tubings,
- having pets in contact with the pump and tubings, which could cause damage.
- Your child can return to school or daycare if otherwise well. If necessary, discuss your child’s equipment, care and feeding needs with school or daycare staff. Discuss your child’s return to school or daycare with your healthcare team.
- Your child can be placed on his or her stomach for play and placed in a baby carrier or car seat.
Travel and transportation
- Always bring with you the equipment needed to administer enteral nutrition and medications when you are not at home, including a “troubleshooting kit” in case of complications. This equipment contains at least:
- the nutritional formula (with ice packs if necessary) or the ingredients required to prepare it,
- medications and a device to crush tablets to powder, if necessary,
- an oral/enteral feeding syringe or feeding bags,
- an oral/enteral syringe (to administer medication),
- an oral/enteral syringe (for irrigation or flushing, after medication administration or feeding),
- two button extension sets, if applicable,
- the enteral feeding pump and backpack, if applicable,
- the power cable for wall outlet, if necessary,
- a spare nasogastric tube, gastrostomy balloon button or tube for replacement,
- two urinary Foley™ catheters, if your child has a stoma: one the same size and one smaller than your child’s tube or button,
- water-soluble lubricant,
- a syringe (for the button balloon or urinary Foley™ catheter),
- a thin protective bandage, if appropriate,
- adhesive bandages,
- water (for irrigation),
- towels.
- Always have an up-to-date list of materials and equipment needed in the travel bag; replace used or missing items. Confirm the frequency of checking expiry dates and equipment status with your healthcare team.
- Keep the specific instructions of the enteral pump used by your child, if applicable, handy.
- Keep a resource list close at hand with the names and telephone numbers of hospital, doctors, other members of your child’s healthcare team and equipment providers. Make sure you know how to contact these resources outside of regular hours and during vacations.
- Before leaving on a trip:
- always check with your insurance company to see if travel to your destination is covered;
- check that the appropriate voltage for the enteral feeding pump is available at your destination;
- make sure you have a document from your healthcare team describing your child’s condition and your child’s needs regarding enteral nutrition along with a complete list of medications;
- bring enough supplies to last for the duration of the trip and add a bit extra as a reserve;
- be aware of the presence of suppliers and other resources that may be required while traveling to or from the destination, in case there is equipment breakdown or other health need;
- plan what to do in case of an emergency (eg, unintentional removal of the tube or button that you cannot change yourself, broken pump, lack of nutritional formula).
- For travel by airplane:
- contact the airline company to inquire about their policy concerning the transport of equipment and formula;
- keep all equipment, formula, medications and documents from your healthcare team with you in the cabin.
- While traveling: make sure the battery of the enteral feeding pump is fully charged.
- Discuss with your healthcare team the possibility of using an alternative method of feeding (push, gravity) while traveling.
Others
Oral stimulation:
- Even if your child’s feeding is partially or not at all possible through the mouth, stimulation of the lips, gums and tongue is important for speech development and to maintain a normal feeling of touch, temperature and taste.
- You can encourage your child to develop these skills by:
- Playing with toys and objects of different sizes and textures that are appropriate for age and developmental level and intended for use in the mouth (eg, sponges, terry towels, rubber toys, small soft toothbrushes),
- Playing with cold rattles or cooled teething toys to stimulate the inside of the mouth,
- Using a pacifier during feeding sessions so that sucking can be combined with the pleasure brought by the food.
- As your child grows older, find more opportunities for sucking and chewing. Oral stimulation should always be pleasant and safe.
- Maintaining this type of stimulation can help prevent your child from developing an oral aversion (not wanting to put anything near the mouth or lips, gagging easily).
- Depending on certain conditions, some children may need more specific techniques or exercises. Discuss this with your healthcare team.
Care of feeding tubes and buttons:
- COMMON care for all types of tubes and buttons:
- Checking the location of the tube or button is essential to ensure that it is used safely (to avoid administering the formula or medication in the wrong place). Several methods are used (eg, measuring external length, checking for stomach contents, checking pH, etc.). Confirm the most appropriate methods for your child’s situation with your healthcare team.
It is essential to verify the correct location of the tube or button in all of the following circumstances:- after installing a nasogastric tube, gastrostomy balloon button or tube (the healthcare team will check the location of other types of tubes and buttons when they are installed),
- before using them (feeding session, medication administration),
- every 4 hours if your child is receiving continuous feeding,
- if your child has certain symptoms (eg, difficulty breathing, coughing, choking, vomiting, reflux, discomfort during feeding, etc.),
- if there are signs that the tube or button is displaced (eg, change in the length of the outer portion of the tube or button stem, detachment of the adhesive bandage or other fastening system, etc.),
- daily, if the tube or button is not used on a regular basis,
- if the tube is blocked, leaking or at the request of your healthcare team.
- Irrigation of the tube and button is very important to maintain proper functioning and to avoid blockages (eg, removing traces of formula or medication). Never irrigate the button directly with a syringe as this may damage the anti-reflux valve; always connect an extension set to the button.
It is essential to irrigate the tube or button in all of the following circumstances:- after installing a nasogastric tube, gastrostomy balloon button or tube,
- before and after use (feeding session, medication administration)
- in-between the administration of each medication,
- after aspirating gastric contents to check the pH,
- every 4 hours during continuous feeding,
- daily, if the tube or button is not used on a regular basis,
- in all other circumstances, at the request of your healthcare team.
- Checking the location of the tube or button is essential to ensure that it is used safely (to avoid administering the formula or medication in the wrong place). Several methods are used (eg, measuring external length, checking for stomach contents, checking pH, etc.). Confirm the most appropriate methods for your child’s situation with your healthcare team.
The quantity and type of water used for irrigation (eg, tap water or cooled boiled water) depends on the model of tube or button (including the extension set) and on the child (eg, age, health condition, etc.). Always follow the instructions of your healthcare team. Each irrigation should be done with the smallest amount of water recommended to prevent the tube or button from becoming blocked.
Other solutions may be recommended for irrigation if the button/tube becomes blocked.
The same care recommendations apply to the urinary Foley™ catheter (until it is replaced by a button or a enterostomy long tube).
- SPECIFIC care for nasal tubes:
- Before each use: Monitor the condition of your child’s nostrils and check that the reference point is always in the same place on the tube.
- Every day: Perform nasal hygiene and check that the dressing securing the tube is clean and securely in place; change it if necessary.
- SPECIFIC care for buttons and enterostomy long feeding tubes:
- NEVER INSTALL OR REPLACE THE BUTTON OR LONG TUBE IF YOUR CHILD HAS A STOMA FOR LESS THAN 6 TO 8 WEEKS (or other length of time as recommended by your healthcare team) as the stoma is not fully healed; all re-insertions in this time period are the responsibility of your healthcare team.
- It is normal for a small amount of yellowish or brownish secretions to come out of the stoma.
- Keep the stoma site as open to air as possible, unless a dressing is recommended by your healthcare team (eg, heavy drainage).
- Every day:
- Clean the skin around the stoma with a small washcloth soaked in room temperature tap water and unscented mild soap (eg, “Dove”). Start on the inside (the area of skin closest to the stoma) and clean outward (the area of skin furthest from the stoma).
- Gently lift the button or the long tube external bolster and clean the ostomy site in the same manner. Secretions may become crusty as they dry. You can easily remove them with a cotton swab. Rinse and dry the skin well.
- If your child has a stoma for less than 6-8 weeks (or other length of time as recommended by your healthcare team), check with your healthcare team to see if the cleaning should be done with saline solution. Refer to your healthcare team for the recipe and storage of homemade saline solution.
- After removing the cover, clean the feeding port of the button or tube with a cotton swab soaked in soapy water to remove any remains of formula. Also clean the anti-reflux valve on the button that is accessible when you open the feeding port. Close the cover tightly.
- Observe the condition of the skin around the stoma; it should be clean, dry and intact (same appearance as usual: similar to the color of the belly or a little pinkish). Check for signs of infection (redness, tenderness, swelling, discharge different from the usual yellowish or brownish discharge, bad odor).
- Check that there is not too much tension on the long tube and that the external bolster is well adjusted to the abdominal wall, as directed by your healthcare team.
- As recommended by your healthcare team, gently rotate the gastrostomy/jejunostomy button to check for mobility and avoid skin irritation.
- Never turn the gastrojejunal button as you could move the portion that is in the jejunum.
- Check with your healthcare team for specifics for gastrostomy and jejunostomy tube care.
- After each feeding session (or minimally every day if the tube or button is not used on a regular basis):
- Observe the condition of the skin around the stoma; it should be clean, dry and intact (same appearance as usual: similar to the color of the belly or a little pinkish). Check for signs of infection (redness, tenderness, swelling, discharge different from the usual yellowish or brownish discharge, bad odor).
- Check if there is any leakage of milk or nutritional formula; if so, place a compress under the button or the external bolster of the tube to absorb it and protect the skin; change the compress as soon as it is wet to keep the skin clean and dry. Discuss this with your healthcare team.
- Weekly for balloon models but only after 6 to 8 weeks following surgery (or other duration as recommended by your healthcare team): Check the amount of water in the balloon to ensure that there are no leaks and that the balloon is functioning properly.
- Connect the specific syringe for this purpose into the balloon port.
- Remove all water and discard. The water may not be colourless.
- Inject the required amount of water into the balloon.
- It is normal to take out a little less water than the amount you put in initially. The water may have evaporated from the balloon. If the difference is more than 0.5 ml, the balloon may be defective.
- If there is not enough water in the balloon when you try to deflate it, inject the usual amount of water into the balloon. Wait 3 to 4 hours and then try to remove the water. a) If the amount has not changed, check after a few days to make sure the balloon is working properly. b) If the balloon is empty, the balloon is probably broken; the tube or button needs to be changed.
Preparation of medications for enteral administration
- Refer to your healthcare team for specifics regarding the preparation and expiration date of medications.
- Medications should always be given in liquid form to avoid blocking the tube or button:
- Use the liquid form of the medication if available.
- If the medication is in tablet form, check with your healthcare team to see if you can crush it into a fine powder and mix it with a little water.
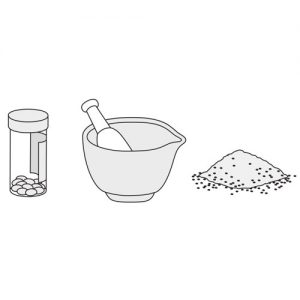
-
- If the medication is in a capsule, check with your healthcare team to see if you can open it and mix the contents with a little water.
- Coated or extended-release medications cannot be crushed as this may interfere with their effectiveness.
- Never mix medications with the formula to prevent them from reacting with each other and clogging the button or tube.
- Never mix medications in the same syringe. Give one medication at a time.
Frequency of equipment replacement:
- Follow your healthcare team’s recommendations about how often equipment should be replaced.
- Any part must be changed if it appears damaged or does not function properly (eg, breakage, color change, stains, rigidity, etc.).
Maintenance and cleaning of material and equipment:
- Always refer to the manufacturer’s recommendations and those provided by your healthcare team if they are different from the following. Your healthcare team will be able to take various factors into consideration (eg, your child’s health condition, comfort, safety, environment, etc.) to provide specific advice for the cleaning and maintenance of materials and equipment.
- Proper cleaning and quick rinsing after use prevents milk or formula remains from drying and accumulating in the equipment.
- We suggest the following way of cleaning the equipment that can be used as a general guide:
- Always wash your hands before starting.
- Disassemble all equipment (bag with tubing, extension set, syringe body and plunger, etc.).
- Always clean and rinse with lukewarm water as hot water can damage the quality of the plastic: it can make it stiff, erase the numbers on the syringes and make the plungers sticky.
- Never use bleach, alcohol, alcohol-based products, peroxide or strongly scented products to clean the equipment. These products can damage the equipment.
- Do not put any parts in the dishwasher.
- After each feeding session:
- Rinse each piece with warm tap water. Make sure the draining water runs clear (no residue).
- Bags and tubing: Use a bottle brush to clean the inside of the bag. If gravity feed: Hang the bag from a hook or the IV pole to clean the tubing; stand over the sink or a large bowl; put 500 ml of warm water in the bag and run it through the tubing until it is clean.
- If pump feeding: leave the tubing in place in the pump; refer to your healthcare team’s or manufacturer’s instructions for rinsing the tubing.
- Extension sets: Fill a syringe with warm water, connect it to the extension set and inject water through the ports until drains out clearly.
- Drain and air-dry all parts on a clean cloth and place them so that the water drains well; air dry the tubing and the hanging bag without the cap on.
- Reassemble the pieces when they are completely dry. Make sure that the black rubber tip of the plunger is completely dry before putting it back into the syringe barrel; otherwise, it may stretch and crack and the syringe will be unusable.
- Store unused equipment in a clean container with a lid until the next use.
- Every day or more often, if necessary:
- Prepare soapy water: 15 ml of dishwasher soap diluted in 125 ml of boiling water. Let it cool before using it.
- Bags and tubing: Put 250 ml of warm water and 1 ml of soapy water in the bag. Use a bottle brush to clean the inside. Run the water through the tubing to clean it.
- If residues remain stuck to the walls of the bag, tubing or nasogastric tube or if odours persist: fill with a solution of 1/2 white vinegar – 1/2 warm tap water. Let stand with the solution in a sink or other container for 10 minutes; then empty the contents of the bag, tubing and nasogastric tube; rinse with clear warm water at least twice to remove any vinegar odour.
- Extension sets: Clean with a syringe of soapy water diluted with warm water; roll the extension set between your fingers to dislodge any sticky residue; thoroughly clean the inside of the feeding and medication port.
- Syringes: Clean the body and plunger with soap and water diluted with warm water.
- Thoroughly rinse all parts with warm tap water until the return water is clear (no soap residue); repeat this rinse as many times as necessary.
- Pay special attention to the connection points.
- Drain and air-dry all parts on a clean cloth and place them so that the water drains well; air dry the tubing and hanging bag without the cap on.
- Reassemble the parts when they are completely dry; make sure that the black rubber tip of the plunger is completely dry before putting it back into the syringe barrel; otherwise, it could stretch and crack and the syringe would be unusable.
- Store unused equipment in a clean container with a lid until the next use.
- When changing the nasogastric tube: fill a syringe with warm soapy water and inject the water into the tube until it comes out clear.
- If formula is given continuously, clean the equipment before adding formula to the bag; some families find it advantageous to use a second bag (eg, when one bag is cleaned, the second bag can be set up to continue enteral feeding).
- The following are specific recommendations for the maintenance and cleaning of the enteral pump after each feeding session:
- Unplug the pump from the electrical outlet before cleaning.
- Clean the exterior surface with a damp cloth.
- Check with the manufacturer or your healthcare team for maintenance and cleaning specifications for the interior.
- Clean the outside of the power cord thoroughly with a damp cloth.
- Never immerse the pump or power cord in water or any other cleaning solution.
- Make sure all parts are dry, including the power cord, before reconnecting the pump.
- Your healthcare team will advise you of the procedures for periodic inspection of the pump (recertification/recalibration) to ensure proper operation and safety.
Charging the enteral pump:
- The pump can be recharged in different ways:
- by electricity in a wall outlet or in a power strip extension equipped with a circuit breaker,
- by an integrated rechargeable battery, if present in the device.
- Do not plug the unit into a wall outlet controlled by a wall switch.
- It is not recommended to use a portable charger (eg, power bank) to operate the pump.
- When a battery is used, make sure it is sufficiently charged for the expected operating time of the pump.
Emergencies:
- Always have a telephone nearby in case of an emergency. Make sure your cell phone is charged at all times.
- Make sure that the pump, if used, is always charged.
- Have the necessary equipment available in case of a power failure (eg, ice-packs and cooler for the formula).
- Have the equipment available to administer the nutritional formula or milk and medications by push (feeding syringe) or gravity (gravity feed bag with tubing) in the event of a problem with the pump (eg, malfunction, inability to recharge).
- Keep a resource list close at hand with the names and telephone numbers of hospital, doctors, other members of your child’s healthcare team and equipment providers. Make sure you know how to contact these resources outside of regular hours and during vacations.
Accident prevention:
- Do not use over-the-counter medications without a doctor’s advice.
- Never leave your child alone during the feeding session; it is important to check that your child is tolerating the formula, is not vomiting, is not accidentally disconnected, etc.
- Attach and secure the tube or button extension set as directed by your healthcare team.
- Make sure the tubing is out of your child’s reach (eg, under clothing) during gravity or pump feeding; if your baby pulls on the tube often, cover the hands in mittens or socks.
- Verify the correct location of the tube or button at these times:
- after installing a nasogastric tube, gastrostomy balloon button or tube (the healthcare team will check the location of all other types of tubes and buttons when they are installed),
- before use (feeding session, medication administration),
- every 4 hours during continuous feeding,
- if your child has certain symptoms (eg, difficulty breathing, coughing, choking, vomiting, reflux, discomfort with feeds etc.),
- if there are signs that the tube or button is displaced (eg, change in length in the outer portion of the tube or button stem, detachment of the adhesive bandage or other fastening system, etc.),
- daily, if the tube or button is not used on a regular basis,
- in all other circumstances, at the request of your healthcare team (eg, blocked tube).
- If your child moves around with an IV pole supporting the bag with or without the pump, it is important to make a few changes around the house to avoid obstacles (eg, move some furniture to provide more space, attach a ramp to allow easy access to the bathroom, remove carpets).
Infection prevention:
- Always wash your hands before providing care to your child and have your child wash his hands before and after all meals and frequently during the day.
- Properly clean the work surface for preparing the milk or nutritional formula to be administered.
- Refer to the section “Conservation of the nutritional formula” to avoid contamination of the food given and the development of infections in your child.
- Follow your healthcare team’s recommendations on how often to change the equipment used at home.
- Make sure to clean and maintain the equipment and materials as recommended. Discuss special cleaning and maintenance measures if your child is immunosuppressed.
Daycare and school:
- Your child’s healthcare team will evaluate your child’s needs and will support you in the planning of integration to daycare or to school.
- Advise school staff of the treatment and care that your child requires.
Additional information and tips can be found on the following sites:
https://www.feedingtubeawareness.org