Clothing
If your child has a tracheostomy, refer to the appropriate section to complete the information.
Bathing and swimming
If your child has a tracheostomy, refer to the appropriate section to complete the information.
Bath:
- Discuss with your healthcare team the option to have longer tubing in the ventilation circuit to facilitate bathing.
- Keep the ventilatory assistance device as far away as possible from the bath to protect it from water splashing.
Facial care:
- Check your child’s skin daily, especially at the points of contact of the mask to the face, if applicable. In particular, check the bridge of the nose where skin breakdown may occur.
- Gently clean the skin, avoid rubbing and pat gently to dry.
- Avoid hot water and scented soaps which may dry or irritate the skin.
- Hydrate facial skin by applying a moisturizer as needed; this may help keep the skin soft and supple.
- Make sure the skin is dry before putting the ventilation mask on your child.
Mouth care:
- It is important to clean your child’s mouth at least twice a day.
- If your child has no teeth, use a small face cloth or a gauze dampened with water and rolled around your index finger, to gently rub your child’s gums front to back.
- Once teeth start to appear, it is important to brush your child’s teeth after each meal and at bedtime. If your child does not eat by mouth, brush the teeth twice daily. Since young children have a tendency to swallow toothpaste instead of spitting it out, use only the size of a small grain of rice in children under 2 years old and the size of a small pea in children up to 6 years old. Use this time to also gently massage their gums with the toothbrush.
- As your child matures, teach and supervise brushing of the teeth.
- Apply, if required, a hydrating product for the lips if they are chapped and dry.
Nose care:
- In all children, secretions, along with bacteria and viruses collect in the nose. Keeping your child’s nose clean helps prevent lung infections.
- If your child is incapable of blowing his/her own nose effectively, saline drops will be helpful to keep the nose clean.
- Refer to your child’s healthcare team for the technique and the frequency of nasal care recommended for your child, including the procedure for the preparation of homemade saline solution and safe storage.
Swimming:
- Discuss with your healthcare team whether it is possible for your child to swim or not.
- If swimming is permitted, then discuss the addition of longer tubing in the ventilation circuit with the healthcare team.
- Keep the ventilatory assistance device as far away as possible from the water to protect it from splashing.
Sleeping
- Position the circuit tubing towards the head of the bed to prevent it from curling, bending getting stuck underneath the child.
- Avoid pulling the tubing or putting tension on the mask to prevent air leaks around the mask.
- Avoid pulling on the tubing or putting tension on the connection to the tracheal cannula to reduce the risk of tracheal injury, accidental decannulation and/or air leakage.
- Ensure that the pillow does not block the exhalation valve mask.
- If a heated humidifier is used, install the ventilatory assistance device as close as possible to the bedside, preferably at a level lower than or equal to the head of the child so that excess condensation, if any, will flow into the water chamber and not into the child’s mask.
- If your child has a tracheostomy, refer to the appropriate section to complete the information.
Nutrition and hydration
- It is not recommended for your child to eat or drink while wearing a mask, in order to reduce the risk of choking. Refer to your child’s healthcare team for specific recommendations.
- Ensure adequate hydration; this hydrates the airway passages (nose, throat) and optimizes your child’s comfort.
- If your child has a tracheostomy, refer to the appropriate section for further information.
Activities
- Your child may participate in daily activities according to ability, endurance and underlying conditions. Discuss with your child’s healthcare team.
- Position your child in the most comfortable position possible to facilitate breathing.
- If your child has a tracheostomy, refer to the appropriate section to identify activities which should be avoided.
Travel and transportation
- Always have on hand a travel bag for all trips outside the home. This bag should contain, at least:
- ventilatory assistance device with:
- the power cable for electrical wall outlet
- a fully charged built-in battery (if present)
- cable with a 12 volt car adapter, if necessary
- an external spare battery with the appropriate cables, if present and if necessary
- two circuits for the ventilatory assistance device (one extra in reserve)
- two interfaces (including a spare)
- ventilatory bag for manual ventilation with the appropriate face mask
- demineralized water for the humidifier, if needed
- a second ventilatory assistance device as a back-up, if necessary.
- ventilatory assistance device with:
- Always have an up-to-date list of the contents of the travel bag to reduce the risk of missing items. Confirm with your healthcare team how often you should verify supply and status of equipment and materials, including expiry date for demineralized water.
- Keep a resource list close at hand with the names and telephone numbers of hospital, doctors, other members of your child’s healthcare team and equipment providers. Make sure you know how to contact these resources outside of regular hours and during vacations.
- During the winter months, always heat up the car interior before placing your child in the vehicle.
- Before leaving on a trip:
- contact your healthcare team to plan travel with ventilatory assistance devices;
- ensure with your insurance provider that travel outside of your home region is covered;
- verify that the electrical voltage required for the ventilatory assistance device is available at your destination;
- make sure you have a document from the healthcare team describing your child’s condition and your child’s needs regarding ventilatory assistance (ventilator parameters) and a complete list of medications;
- have on hand a recent height and weight for your child and the specific sizes of all equipment;
- bring enough supplies to last for the duration of the trip and add a bit extra as a reserve;
- make sure to ask if equipment providers and other resources are available at your destination in the event of equipment failure or other healthcare needs;
- take the climate of your destination into consideration because the relative humidity of the ambient air could modify the level of humidity necessary to adequately hydrate your child’s airway passages.
- During your travels:
- ensure that the battery of the ventilatory assistance device is fully charged;
- remove the heated humidifier if the ventilatory assistance device is used while the child is mobile; if your child has a tracheostomy, replace the heated humidifier by an artificial nose during transportation;
- always empty the water chamber of the heated humidifier before packing it in the storage bag.
- For travel by airplane:
- contact the airline company to inquire about their policy concerning the transport of medical equipment;
- keep all medical equipment and supplies, medications and documents with you in the cabin.
- If your child has a tracheostomy, refer to the appropriate section to complete the information.
Others
Cardio Pulmonary Resuscitation (CPR): Make sure that you and all persons responsible for your child’s care are trained. Consult your child’s healthcare team regarding referral to pertinent resources and the frequency of training renewal required.
Emergencies:
- Always have a telephone nearby in case of an emergency. Make sure your cell phone is charged at all times. When you go out, bring what you need to charge the phone, when necessary (cable with charger and portable Power Bank charger).
- During the time that your child is receiving ventilatory assistance, your child should always be monitored by a trained and competent individual capable of intervening, as needed. Some children require increased supervision due to their specific needs; discuss with your child’s healthcare team.
- Outside of the time that your child receives ventilatory assistance, your child should have access, at all times, to a trained and competent individual who is able to assess your child’s respiratory status and intervene as required (eg, aspirate secretions, start ventilatory assistance earlier than planned).
- If your child has a tracheostomy, refer to the appropriate section to complete the information.
Humidity:
- Air entering the nose and passing through the throat (pharynx) is filtered, warmed and moistened by the airways before reaching the lungs. As your child receives ventilatory assistance, air is pushed into the lungs by the device at high flow rates; the body’s “natural” humidification system may be insufficient. Thus, air must be warmed and moistened to prevent dryness and irritation of lining of the airways. Excessive dryness causes irritation which may result in nosebleeds, nasal congestion, and increased production of secretions. Secretions may be thick, sticky and difficult to clear; this increases the risk of respiratory infections.
- Lack of humidity can also cause discomfort and make the ventilatory assistance more difficult.
- Avoid extremes of temperature (hot or cold) which may cause condensation in the ventilation circuit tubing.
- The recommended relative humidity in the home, measured with a hygrometer, should be between 40 to 50%.
- If your home air is too humid (55% and more), install a dehumidifier and clean it every week in order to prevent the presence of mold in the air that your child breathes.
- If your home air is too dry (less than 40%), the following daily habits can help increase the moisture in your home:
- do not activate the exhaust fan when you cook or boil water;
- avoid using an air conditioner in the summer;
- keep the bathroom door open when you shower;
- minimize the use of electric heaters, wood burning stoves and fireplaces during the winter;
- eliminate carpeting and rugs in the home.
- For a child receiving invasive or non-invasive ventilation, the level of air humidity should be increased at night and as often as possible during the day; this is accomplished by connecting the ventilatory assistance device to a heated humidifier. During the day, an artificial nose may replace a heated humidifier only in an invasive ventilation circuit.
- Water chamber of the heated humidifier in the ventilatory assistance device:
- It is essential to use distilled or demineralized water in the water chamber of the humidifier. Tap water or bottled water contains minerals which can form limestone scale in the bottom of the water chamber. This scale is difficult to remove and particles from the limestone may irritate your child’s airways and lungs.
- Change the water in the water chamber every day. If there is water left in the water chamber at the end of the day, discard it. Rinse the water chamber with tap water and refill it with distilled or demineralized water. The daily rinsing of the water chamber prevents growth of bacteria and mold.
- If the ventilatory assistance device is used several times a day, then the water in the water chamber is good for period of 24 consecutive hours. Make a habit of rinsing the water chamber and changing the water at the same time of day.
- Do not add scented products or decongestants to the water. These products may irritate your child’s airways and damage the water chamber.
- Discuss with your child’s healthcare team ways to improve the humidity; this will improve your child’s comfort and keep secretions loose for easier clearance.
- If your child has a tracheostomy, it is even more important to ensure adequate humidity because inhaled air bypasses the nose and throat where natural humidification usually takes place; refer to the appropriate section for more details.
Air quality:
- Avoid all exposure to traditional or electronic cigarette smoke or vapour, especially at home.
- Clean and regularly change filters on the air conditioners.
- Make sure that the air around your child and the ventilatory assistance device is free of dust and smoke.
- In your child’s proximity, avoid:
- accumulation of dust, presence of rugs, upholstered furniture and home accessories that are difficult to clean (eg, heavy drapery),
- dust from renovations,
- wood burning heating systems (stove or fireplace),
- excessive pollution (eg, smog, heavy traffic, strong winds).
- In your child’s room:
- avoid the presence of toys and stuffed animals in your child’s bed,
- use pillows cases, sheets, and blankets made of washable synthetic material (hypo-allergenic),
- avoid sheets that are very soft and fluffy with fibres (eg, flannel sheets) are not recommended: they attract dust,
- wash bedding in hot water every week in order to destroy dust mites,
- dry bedding in a dryer if your child is allergic to pollen.
- If your child has a tracheostomy, refer to the appropriate section for further information.
Prevention of infections:
- Always wash your hands before providing care to your child and have your child wash his hands before and after all meals and frequently during the day.
- If you have a cold, the flu or another respiratory infection, use non sterile gloves and wear a mask when providing care to your child.
- Be sure to clean and maintain equipment and materials as recommended.
- If your child has a tracheostomy, refer to the appropriate section for further information.
Power supply for the ventilatory assistance device:
- Ventilatory assistance devices can be powered in different ways:
- by electricity directly from a wall outlet; if direct access to an electrical outlet is impossible, then a multisocket extension cord with circuit breaker can be used,
- by a built-in rechargeable battery, if present,
- by an external battery with the appropriate cables, if present,
- by a cable with a 12 Volt adapter for connection in a car.
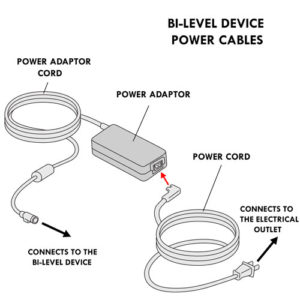
- The power cables of the bi-level devices have two parts: a power cord which connects the power adaptor to the electric wall outlet and a power adaptor cord which connects the power adaptor to the bi-level device.
- If a battery is used, make sure that there is an adequate charge for the predicted duration of ventilatory assistance.
- It is not recommended to use a portable power bank to operate the ventilatory assistance device.
- The electrical wall outlet should be clearly visible and easily accessible. At home, identify the fuse or circuit breaker that is connected to this electrical outlet.
- Do not connect the device to an electric outlet that is controlled by a wall switch.
- Ensure that one or more external batteries (if present) are fully charged at all times.
Installation of the ventilatory assistance device:
- The device must always be installed in a clean, well-ventilated, dust-free room.
- The device should be placed on a firm, level surface that is at the same height as your child’s head or slightly lower.
- Arrange the device so that the power cable is not in the way of foot traffic.
- The device should be placed away from any heating or cooling equipment (eg, radiator), direct sunlight, cold drafts and any device which emit electromagnetic waves (eg, cell phone, tablet, cordless telephone base, microwave, etc.).
- Air must be able to flow freely around the device so that it works properly.
- Make sure that there are no soiled, wet or moldy items near the air inlet of the device (eg, plants, curtains or stuffed toys, etc.).
- Avoid exposing the device to extreme temperatures (hot or cold) and ensure that it is protected in case of rain or snow.
- If a heated humidifier is used, install the ventilatory assistance device as close as possible to a bedside table, preferably at a level lower than or equal to your child’s bed to ensure that any excess condensation stays in the water chamber and not in the face mask.
- If the heated humidifier is not integrated in the ventilatory assistance device, it should be installed in one of the following ways to stabilize the humidifier: on a roller stand or on a table stand.

- If the device is used while your child is in a wheelchair, remove the heated humidifier and store it in a suitable transport bag, securely attached to the wheelchair.
Equipment replacement frequency:
- Refer to your healthcare team or the manufacturer’s recommendations for the replacement frequency of the parts of the ventilation circuit, the interfaces and all other required equipment (eg, filters, water chamber, chin rest, etc.).
- Any equipment must be changed (eg, tubing, mask, water chamber), if you notice that it is worn or damaged (eg, cracks, colour change).
Maintenance and cleaning of medical supplies and equipment:
- Always refer to the manufacturer’s recommendations and those provided by your healthcare team. There may be certain recommendations for the cleaning and maintenance of equipment based upon the unique features of your child (eg, health condition, comfort, safety, living environment, etc.).
- A general guide for the cleaning and maintenance of equipment is as follows:
- Always wash your hands before starting.
- Prepare the sink: wash it, disinfect it with bleach and then rinse thoroughly with running tap water or use a large bowl reserved only for the cleaning of your child’s medical equipment.
- Disassemble all the equipment (according to your child’s healthcare team’s recommendations) so that all the parts can be cleaned thoroughly.
- Rinse all the parts under warm tap water so as to remove any debris (eg, secretions, saliva, blood).
- Soak all parts in a sink or in a dish washing bin filled with warm water and non-perfumed, non-antibacterial dish soap, (eg, Sunlight) for 10-15 minutes.
- Never use bleach, alcohol or non-diluted hydrogen peroxide to clean equipment; these products may damage the equipment.
- If needed, brush the interior and exterior of the parts that remain soiled with a soft baby bottle brush.
- Rinse all parts with warm/hot water. Hot water may damage certain equipment.
- Shake off as much excess water as possible from items that have been rinsed.
- Allow all parts to dry on a clean towel placing them in such a fashion that will allow water to drain away from them.
- Reassemble all components once thoroughly dry.
- Store the equipment that is not in use in a bag used only for this purpose (eg, cotton pillowcase) that will protect the equipment from dust and dirt, according to your child’s healthcare team recommendations.
Here are further recommendations for specific equipment in addition to the general guidelines described above:
- Mask:
- daily:
- Clean the inner surface including the inside cushion of the mask using a damp cloth soaked in mild soap and water. All traces of face oil must be removed from the mask so that it continues to fit properly.
- If the exhalation valve is dirty, clean it with a soft bristle brush according to the guide above.
- Inspect the mask and straps for signs of wear and tear.
- each week: Disassemble the mask and the straps according to your child’s healthcare team recommendations; soak them to clean using the guidelines above.
- daily:
- Mouthpiece:
- daily: Clean the surface with a damp cloth soaked in mild soap and water.
- each week: Clean according the guide above.
- Tracheostomy adapter:
- each week and more often if needed (eg, soiled with accumulation of saliva or secretions): Clean using the general guide above.
- Ventilatory assistance device:
- Outside surface: Clean the outside surface using a damp cloth once weekly; allow to dry.
- Unplug the device before cleaning and check that it is dry before reconnecting it to an electrical supply.
- Handle the device carefully to avoid damage. Always remove the water chamber prior to cleaning to prevent water leaking into the device.
- Do not immerse the device or the power cables in water; keep the device dry.
- Filter: Clean and maintain according to the manufacturer’s recommendations.
- Humidifier:
- Clean the outside surface weekly with a damp cloth and let dry.
- The heating element of the humidifier may be hot; let it cool for at least 10 minutes before cleaning.
- Water chamber:
- daily:
- Change the water in the water chamber every day. If water remains in the water chamber at the end of the day, discard it. Rinse the water chamber with tap water and refill it using distilled or demineralized water.
- Do not use tap water or bottled water to refill the water chamber.
- each week:
- Clean using the general guide above.
- Some models can be cleaned in the dishwasher; refer to the manufacturer’s recommendations.
- If deposits remain in the water chamber, use a dilute solution of water and vinegar to de-scale. Refer to your healthcare team for specific instructions and proportions of vinegar:water to use.
- daily:
- Artificial nose:
- daily and more often if needed (eg, soiled with secretions or water accumulation): Discard and replace.
- Invasive ventilation circuit and non-invasive ventilation circuit with mask:
- each week and more often if needed (eg, presence of blood, secretions): Clean the tubing, dead space, adapter and exhalation valve, if present, according to the general guidelines above.
- each week: Replace the antibacterial filter, if present.
- Circuit for mouthpiece:
- each month: Discard and replace with a new circuit.
- Ventilatory bag and corresponding face mask (specific for use with the ventilatory bag):
- as needed: Clean the outside surface with a damp cloth soaked in mild soap and water.
- Do not immerse the ventilatory bag in water.
Communication:
- In order to speak, a child with non-invasive ventilation must learn to coordinate self breathing with the air flow from the ventilatory assistance device. It is usually easier for children to speak during the expiratory phase of ventilation. Discuss with your child’s healthcare team if needed.
- If you child has a tracheostomy, refer to the appropriate section for further information.
Daycare and school:
- Your child’s healthcare team will evaluate your child’s needs and will support you in the planning of integration to daycare or to school.
- Advise school staff of the treatment and care that your child requires.