Indications:
- The aspiration of tracheobronchial secretions (via the tracheostomy tube) is needed to keep the cannula clear and to remove secretions that accumulate in the trachea if your child is not able to cough effectively. Keeping the cannula and trachea clear of secretions can improve the passage of air in and out of the lungs and help prevent respiratory infections.
- Below is a suggested method that can serve as a guide; discuss the specific type of medical supplies and equipment used for your child with the healthcare team.
Considerations:
- Too frequent aspiration can irritate and damage the fragile lining of the respiratory tract, increasing secretions and the risk of infection. Limit this procedure as required or requested by your child and when your child has any of the following:
- audible or visible secretions at the entrance of the tracheal cannula,
- breathing that is noisy, shallow, more rapid than usual or wheezing,
- obstruction or blockage of the tracheal cannula is suspected,
- decreased oxygen saturation,
- weak cough (ineffective in clearing secretions),
- indrawing (retraction of the skin over, under and in between the ribs) and/or nasal flaring (enlargement of the nostrils during breathing),
- discomfort without obvious cause (eg, continuously crying, agitation, scared look on your child’s face),
- excessive sweating,
- pale skin,
- blue color of lips and nail beds,
- anxiety or agitation,
- refusal to eat or drink.
- Aspiration of tracheobronchial secretions is also indicated in the following situations:
- before tracheostomy care,
- if needed, before changing the tracheostomy ties,
- if needed, after deflating the cuff of the tracheal cannula,
- before and/or after a change of the tracheal cannula,
- before and/or after administration of aerosol medications,
- after using a cough assist technique.
- The pressure regulator on the suction device should be adjusted to the pressure level recommended by your healthcare team so that secretions are effectively removed without damaging the airway lining. In general, the recommended pressure level varies according to the age of the child:
- Infants: between 60 and 80 mmHg
- Children: between 80 and 100 mmHg
- Adolescents: between 80 and 120 mmHg.
- If the secretions are very thick, a higher pressure may be required. To prevent tissue injury, gradually increase the pressure and watch carefully for signs of bleeding or discomfort. Discuss this with your healthcare team.
- The aspiration of tracheobronchial secretions is done with a flexible suction catheter.
- Do not use the catheter used to aspirate oral or nasopharyngeal secretions to aspirate tracheobronchial secretions. This can increase the risk of infections. Use a separate catheter to aspirate tracheobronchial secretions.
- If your child has a fenestrated tracheal cannula and that the internal portion is also fenestrated, then replace the internal portion with a non-fenestrated internal cannula prior to suctioning.
- It is normal for your child to cough during the aspiration procedure.
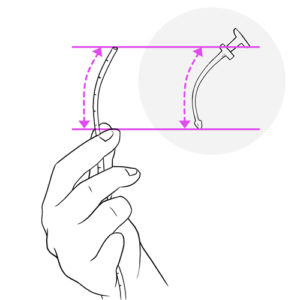
- Catheter insertion length: To avoid inserting the catheter too deeply in the trachea and damaging the fragile lining of the airways, it is important to follow the predetermined maximum insertion length for your child.
- Refer to the technique taught to you by your healthcare team or use this method: Using the tracheal cannula obturator catheter, measure the length of the part of the obturator that fits inside the tracheal cannula, note the distance on the suction catheter, using the measurement markings on the catheter as a guide to determine the reference point.
- If the aspiration is not effective with this predetermined maximum catheter insertion length, then discuss with your healthcare team if a deeper aspiration is required. Deep aspiration can damage the fragile lining of the airways; always consult your healthcare team for recommendations specific to your child.
- If your child has a change in tracheal cannula size, re-measure and verify the maximal catheter insertion length; always check this measurement with the healthcare team.
- Refer to the technique taught to you by your healthcare team or use this method: Using the tracheal cannula obturator catheter, measure the length of the part of the obturator that fits inside the tracheal cannula, note the distance on the suction catheter, using the measurement markings on the catheter as a guide to determine the reference point.
- Installation of saline into the tracheal cannula prior to aspiration of secretions should only be done when recommended by your healthcare team; this may push bacteria further into the lungs, increasing the risk of infection. If saline installation is recommended, follow the instructions of your healthcare team to complete the procedure safely.
- To prevent secretions from your child’s nose, mouth or throat from entering into the lungs and increasing the risk of infection, your healthcare team may also recommend that you first aspirate your child’s nose, mouth and pharynx in certain circumstances such as: changes in position, during deflation of the tracheostomy balloon, etc.
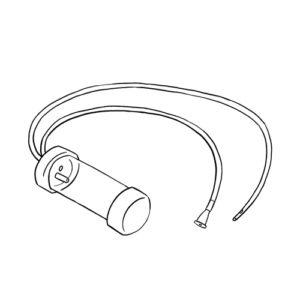
- In an emergency (eg, Power failure) it is possible to use a mucus trap device to aspirate secretions via the tracheal cannula. Always have this device on hand, especially when you are away from home. Refer to your healthcare team to learn how this device works.
- Determine if you require a second person to help hold your child in a secure position (for eg, if your child is young or moving around a lot).
- Good handwashing is essential before and after providing care.
- Ensure the comfort of your child during care by using different positioning and distraction techniques.
Frequency:
- Aspiration of tracheobronchial secretions should be done at least twice daily (morning and bedtime) to keep the tracheal cannula clear. More frequent aspiration may be required depending upon the amount and thickness of secretions, your child’s activity level, your child’s ability to effectively clear secretions by coughing, etc. Verify the recommended frequency of aspiration for your child with the healthcare team.
- If your child has difficulty eating due to secretions, aspirate secretions before meals.
- It is best to wait at least 30 minutes after meals before aspirating secretions to reduce the risk of vomiting.
- Wait at least 30 minutes between aspiration sessions, if possible.
Required materials:
Always have on hand all equipment required in case of emergency.
The methods of care below are illustrated with a LSU suction device.
Refer to your child’s healthcare team if the material, sequence and steps taught to you are different than those described.








