
- Three different types of tracheal cannulas exist (ex: Bivona®, Shiley®, Portex®). The type of cannula selected depends upon the age, size and medical conditions of the child. Your child’s healthcare team will provide you with information regarding the type of tracheal cannula best suited to your child’s condition.
- A simple tracheal cannula is most frequently recommended in children. It is composed of one single tube (cannula) that is inserted into the trachea.
SIMPLE TRACHEAL CANNULA AND COMPONENTS
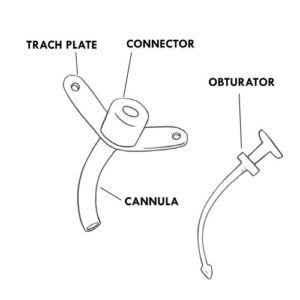
Body of the tracheal tube, commonly called “cannula”
- Portion of the cannula inserted internally into the trachea and therefore invisible externally.
- Helps to keep the tracheostomy open (patent).
- Helps the passage of air in and out of the lungs and facilitates the suctioning of secretions.
Flanges or neck collar or trach plate
- External, visible portion of the tracheal cannula that rests on the neck.
- Openings on each side of the flanges are present to allow for insertion of ties (a Velcro® band or ribbons) that wrap around the back of the neck to hold the tracheal cannula in place.
- Serves as a point of anchor on which to place the fingers and stabilize the cannula when providing care.
Connector
- External, visible portion of the cannula.
- Opening through which air can pass into the lungs.
- Opening through which suction catheters can be inserted into the tracheal cannula.
- Permits the connection of the tracheal cannula to an artificial nose (heat and moisture exchanger), a speaking valve, a ventilatory bag and/or a respirator.
Obturator
- Used when changing a tracheal cannula.
- Serves as a guide during the introduction and proper placement of the tracheal cannula in the trachea.
- The rounded tip allows for a smooth insertion and minimal irritation to the tracheal walls.
- Must be removed immediately once the tracheal cannula is in place because it completely blocks the passage of air.
- Other types of tracheal cannula’s can be used in children.
OTHER TYPES OF TRACHEAL CANNULAS
Cuffed cannula
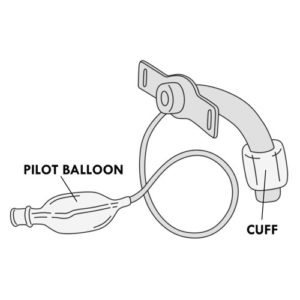
- This type of tracheal cannula includes a soft cuff (invisible on the outside) that goes completely around the end of the simple tracheal cannula or the outer cannula (see the two-piece cannula below). This cuff can be filled with air.
- Included is a pilot balloon, visible on the outside, that indicates if the cuff is filled with air or not.
- When the cuff is inflated with air, it creates a seal between the tracheal wall and the tracheal cannula, blocking (partially or completely) air from leaking through the mouth or the nose.
- When the cuff is deflated, air escapes around the vocal cords allowing the child to speak and in some cases for the child to eat and drink more easily.
- Cuffed cannulas are used mainly in children that require invasive ventilation or to prevent secretions from the nose and mouth from entering the lungs of children at risk for aspiration.
- The pilot balloon allows you to know if the cuff is inflated or not and whether it is properly functioning.
Two piece cannula: inner cannula and outer cannula
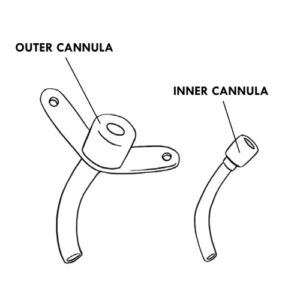
- This larger type of cannula is used mainly in adolescents and adults.
- Composed of an outer cannula (placed within the trachea) and an inner cannula (placed within the external cannula).
- The inner cannula can be locked into the external cannula.
- The inner cannula must be removed and cleaned (if reusable) or changed (if disposable), every day or according to your child’s healthcare team.
Fenestrated tracheal cannula
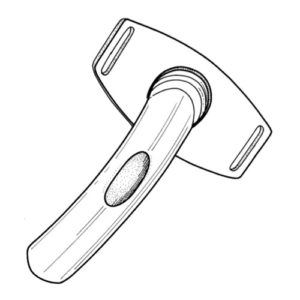
- 2 piece cannula where the external cannula has an opening (fenestration) that allows air to escape through the vocal cords.
- The inner cannula may have a fenestration or not:
-
-
-
-
-
-
-
- the inner fenestrated cannula allows the child to speak;
- the inner non-fenestrated cannula allows suctioning of secretions and ventilation via a respirator.
- Due to their larger size, fenestrated cannulas are rarely used in small children. They may be used in some adolescents.
- The tracheal cannula is held in place by tracheostomy ties (cotton ribbons or Velcro® band) that circle to the back of the neck.
- Specific care must be provided to children with a tracheostomy:
- cleaning of the skin around the tracheostomy and replacement of the tracheostomy dressing,
- replacement of the tracheal cannula,
- replacement of the inner cannula, if a 2 piece cannula is in place,
- suctioning of secretions,
- administration of medication via a tracheostomy,
- invasive ventilation, if needed,
- manual ventilation, if needed,
- cough assistance.
- Depending on your child’s condition, different types of equipment can be used to increase the level of ambient humidity in order to allow your child to make sounds or speak, to deliver solutions and medications to his tracheostomy or to manually assist his breathing.
ADDITIONAL EQUIPMENT
Artificial nose (or filter exchanger or heat and moisture exchanger)
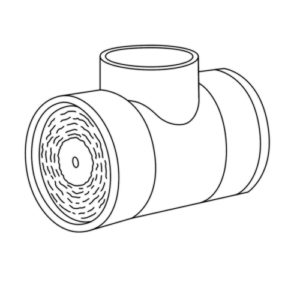
- A device that serves to humidify, warm and filter the air inhaled by capturing the end portion of exhaled air that was humidified and warmed by the lungs.
- Used in children whose condition permits.
- Filters the air inhaled of any particles that may irritate the lungs.
- Some artificial nose models connect to the tracheal cannula while others can be placed in the respirator circuit.
- Can be used at any time but mainly used during the day to facilitate outings particularly in cold temperatures and in areas where there is a lot of dust.
- Useful in protecting the tracheal cannula opening in certain situations (bathing or to protect against the aspiration of small objects).
- Certain models allow connection to oxygen.
- Not to be used with a heated humidifier or nebuliser as this may cause an over-accumulation of humidity which can cause breathing problems.
- An artificial nose is not recommended for nighttime use in children who are on a ventilator; instead an integrated heated humidifier is recommended.
- Must be discarded and replaced every day, or more often, when filled with secretions or water.
Tracheal collar
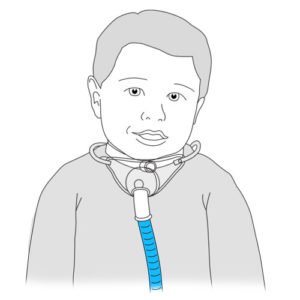
- A device that serves to humidify inhaled air.
- Connected to a large volume nebulizer and an air compressor.
- Used primarily during naps and at night.
- It can also be used to deliver medication or oxygen via a small volume nebulizer.
- Installed over the tracheal cannula and attached around the neck.
- Clean once a week (or more often if needed) with warm non-perfumed soapy water; rinse in warm tap water and let air dry completely before storing in a clean, closed container.
- Replace the tracheal collar every three months or more often if required according to the manufacturer’s recommendations or your child’s healthcare team.
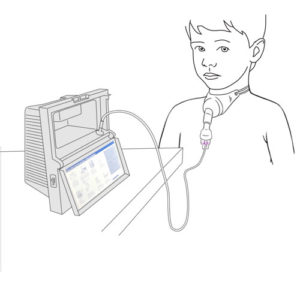
Air compressor for humidity delivery
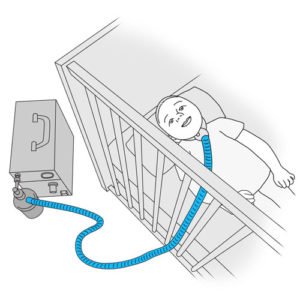
- A machine that allows for the delivery of humidity via a tracheal collar and aids in the prevention of mucus plugs.
- Requires the use of demineralized water in order to avoid harmful calcium deposits that may accumulate when boiled water is used.
- Since this equipment can limit your child’s movements, it is often used at night and during naps.
- The equipment must be well maintained in order to avoid the growth of bacteria or mold. Follow the manufacturer’s recommendations or that of your child’s healthcare team.
Heated humidifier (or heated humidifier plate)
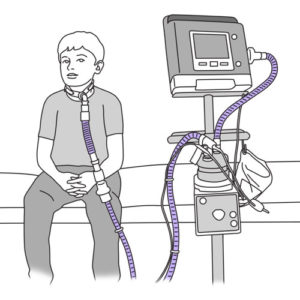
- A device that is integrated into a ventilatory assistance device in order to deliver heated humidity.
- Generates a higher humidity level than an artificial nose, and so is usually recommended at night, during naps and as much as possible during the day.
- Can be used with a tracheal collar or a ventilatory interface.
Speaking valves (ex: Passy-Muir®, Shiley®)
- A device that attaches to the tracheal cannula connector and helps the child to speak, while allowing the continuous passage of air.
- Used in children whose condition permits.
- The one way valve opens during inspiration (air taken in through the tracheostomy) and closes during expiration (air expelled out through the tracheostomy); this causes the exhaled air to be directed past the vocal cords so that the child can speak.
- Increases the ability to swallow.
- Improves the capacity to taste and to smell odors.
- Remove the valve before providing all aerosol therapy treatments.
- If a cuffed tracheal cannula is in place, the cuff must always be deflated before using a speaking valve.
- Clean the valve every day with warm water and a mild non perfumed soap; rinse thoroughly with warm tap water and let air dry completely before storing in a clean, closed container.
- Change the valve if it becomes sticky, noisy, has black residue or if it vibrates even when cleaned regularly.
- Refer to the manufacturer’s recommendations for the duration of use. A well maintained speaking valve should last at least 2 months (Passy-Muir®) or 28 or 30 days (Shiley®).
Small volume nebulizer (or mini nebulizer)
- A device used to provide an aerosol treatment.
- The nebulizer, when connected to an air compressor, aerosolizes medication so that it can easily be inhaled and reach the lungs.
- The nebulizer is attached directly to the tracheal collar or a T piece added to the respiratory circuit that allows the child to inhale the medication.
Metered dose inhaler (MDI) (or pump or puffer) with a spacer (Aerochamber® or air chamber)
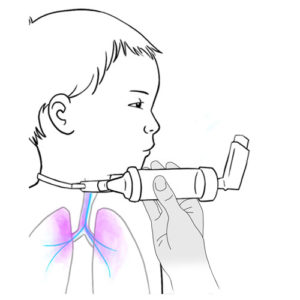
- Provides a metered dose inhaler treatment.
- A metered dose inhaler is a device that delivers medication in the form of an aerosol; it delivers very small particles of medication to the lungs.
- A metered dose inhaler is a metal cartridge inserted into a plastic casing; the medication is contained under pressure in the metal cartridge.
- When the cartridge is pushed downwards, a puff of aerosolized medication is released.
- The use of an in line air chamber, allows for the fine mist of particles (puff) to slow down and accumulate after the cartridge is pushed downwards, so that the aerosolized medication can then be inhaled in a more coordinated, controlled fashion at your child’s own pace.
- Treatment with a metered dose inhaler can be delivered via the tracheal cannula connector or via an in-line ventilator circuit metered dose inhaler adapter.
- The connection and disconnection of these medical devices to the tracheal cannula must be performed with care so as to avoid unnecessary pull or tension on the cannula itself.
- With adequate observation and good daily care, breathing through a tracheostomy is comfortable and safe for your child. Do not hesitate to ask your child’s healthcare team any questions you may have regarding your child’s care needs.