What is it?
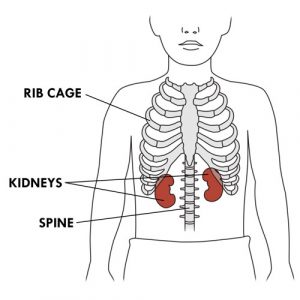
- The kidneys are two bean-shaped organs located on either side of the spine, below the rib cage.
- The kidneys are very important because they perform three essential functions:
- they remove waste products from the blood;
- they regulate the amount of water and certain minerals that the body needs to stay healthy;
- they produce hormones that control other body functions.
- In their elimination function, the kidneys “clean” the blood by removing waste products and excess water and mineral salts that form urine. The kidneys specifically eliminate:
- waste products: Urea is a waste product produced by the breakdown of proteins absorbed from food and creatinine is a waste product produced by muscle use. Some drugs also produce waste products through their breakdown. The elimination of wastes products by the kidneys prevents the onset of many ailments.
- excess water: The body must contain the right amount of fluids to function properly. The kidneys ensure the balance of liquids by keeping the necessary amount of water in the tissues and by removing the surplus. This balance stabilizes the blood pressure and prevents swelling.
- excess mineral salts: Mineral salts (eg, sodium, potassium, calcium, phosphorus) must be present in adequate amounts in the blood and body fluids for the body to function properly. Excess minerals are eliminated by the kidneys to prevent complications (eg, irregular heartbeat, muscle cramps, brittle bones, etc.).
- excess acids: The balance between the acidity and alkalinity of the body (or acid-base balance) is essential to maintain good health. The kidneys play an essential role in maintaining this balance by producing acidic urine (to remove excess acids in the urine) or basic urine (to keep the necessary acids in the blood). This balance contributes to the healthy growth and development of the. The pH of a solution (eg, urine) is a measure of whether it is acidic or basic.
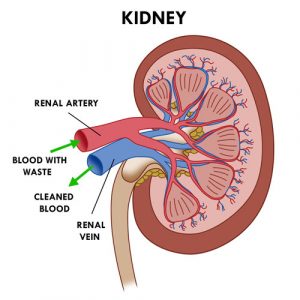
- The elimination function of the kidneys can be imagined as a “washing machine” for the body, where the blood enters “dirty” (with waste) and leaves “clean” (without waste).
- In the production function, the kidneys make hormones. Hormones are substances that circulate in the bloodstream and act as “messengers” to influence certain body functions (eg, control of blood pressure, production of red blood cells and maintenance of adequate calcium levels in the body). More specifically, the kidneys make or help make theses important hormones:
- renin: helps maintain normal blood pressure;
- erythropoietin: stimulates the bone marrow to produce red blood cells and thus avoid anemia;
- calcitriol (active vitamin D): helps to strengthen bones and maintain adequate levels of calcium in the blood. Calcium is necessary to keep bones healthy.
- Let’s get back to the elimination function of the kidneys. The absorption of food through the stomach and intestines produces waste. These wastes end up in the bloodstream. Every minute, about 20% of the total volume of blood in the body flows through the kidneys via the renal arteries. After the kidney filters the blood, the cleaned (or purified) blood then returns to the circulation via renal veins.
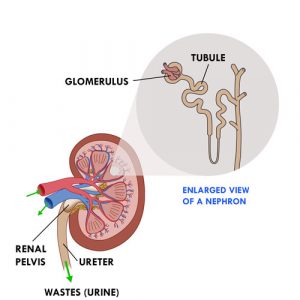
- The cleaning of the blood is done by filtration. Each kidney contains more than a million small units (nephrons). Each nephron consists of a tiny filter, the glomerulus, connected to a small tube (tubule).
- Blood coming from the renal arteries is filtered through the glomeruli, which retain red blood cells and proteins and allow water to pass into the tubules. This is the beginning of urine formation. The good elements (eg, minerals, vitamins, amino acids, glucose, etc.) and most of the water return to the blood from the tubules while the waste products remain in the urine. If some of the good elements are in excess, they are eliminated in the urine.
- The urine formed in the tubules flows into the funnel-like renal pelvis.
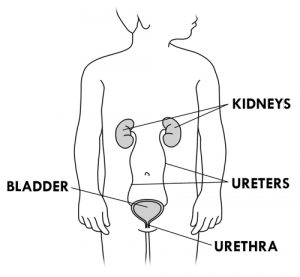
- The renal pelvis extends outside the kidney into a long tube (ureter). Urine leaves the kidneys through both ureters and travels to the bladder, which is a pouch-like storage space. The urine stays in the bladder until the child urinates (pees). Urine leaves the bladder via a small tube (urethra) to the outside of the body.
- When a child drinks a lot of liquids, the kidneys produce and eliminate a lot of urine. On the other hand, when a child loses fluid through vomiting, diarrhea or sweating, the kidneys produce less urine to keep the body’s fluids in balance.
- When the kidneys are not functioning properly, there is a gradual build-up of waste products, minerals and water in the body. There is also a dysfunction in the production of hormones that control blood pressure, red blood cell production and calcium absorption. This is called kidney disease (or kidney failure).
- Kidney disease can be temporary or permanent. It can range from mild to severe and can progress over time. There are two types of kidney disease:
- acute kidney disease: sudden loss of kidney function that can be caused by decreased blood flow to the kidneys, severe dehydration, toxicity (adverse effects) of certain medications, inflammation, or kidney blockage; acute kidney disease is usually temporary and lasts only a few weeks if treated promptly.
- chronic kidney disease (CKD): gradual loss of kidney function (decrease in kidney function for three months or more) caused by a chronic disease; CKD may be mild and remain so, develop very rapidly, or progress slowly over several years; it may also worsen to the point where the kidneys stop functioning completely.
- The main causes of chronic kidney disease in children are:
- congenital abnormalities of the kidneys or urinary tract; eg, malformations with obstruction (blockage of urine) or with reflux (urine that flows back up from the bladder to the kidneys),
- kidney malformations (eg, dysplasia or hypoplasia of the kidneys),
- glomerular diseases/glomerulopathies (eg, glomerulonephritis).
- As the kidneys deteriorate and chronic kidney disease progresses, symptoms vary depending on the severity of the disease:
- fatigue, weakness,
- vomiting, nausea,
- loss of appetite, bad taste in the mouth,
- weight loss,
- swelling of the ankles, hands and eyelids,
- shortness of breath,
- insomnia at night and drowsiness during the day,
- itching,
- muscle cramps.
- Chronic kidney disease (CKD) is divided into stages based on how much the kidneys are functioning and able to filter waste products. Kidney/renal function is assessed by measuring the GFR (Glomerular Filtration Rate). Measuring GFR involves checking the clearance of creatinine, which is the amount of this waste product eliminated by the kidneys.
STAGES OF CHRONIC KIDNEY DISEASE (CKD)
Stage 1: CKD with normal renal function
- Renal function (GFR): >90%
- Symptoms: None
- Treatments:
- Search for the cause
- Medical follow-up
Stage 2: CKD with mild renal failure
- Renal function (GFR): 60-89%
- Symptoms: None
- Treatments:
- Medical follow-up
- Evaluation of the progression of the CKD
Stage 3A: CKD with mild to moderate renal impairment
- Renal function (GFR): 45-59%
- Symptoms: First symptoms may appear
- Treatments:
- Same as stages 1 and 2
- Tests to identify, prevent and treat complications (anemia, bone disorders)
- Treatment of associated diseases
Stage 3B: CKD with moderate to severe renal impairment
- Renal function (GFR): 30-44%
- Symptoms: First symptoms may appear
- Treatments:
- Same as stages 1, 2 and 3A
- Preservation of veins (keep veins n good condition for possible hemodialysis treatments)
Stage 4: CKD with severe renal failure
- Renal function (GFR): 15-29%
- Symptoms: Worsening of symptoms
- Treatments:
- Same as stages 1, 2 and 3
- Discussion of future treatment options
- Continued treatment and monitoring
- Begin evaluation for renal transplantation
Stage 5: CKD with End-Stage Renal Disease (ESRD)
- Renal function (GFR): <15%
- Symptoms: Worsening of symptoms and appearance of new symptoms
- Treatments:
- Depending on the nature of the symptoms and the assessment of the renal function: start of treatment to replace the elimination function of the kidneys
- Registration on the transplant list
- The healthcare team uses a variety of factors to determine the most appropriate treatment for the child with chronic kidney disease:
- assessment of kidney function,
- the nature of the symptoms experienced,
- general health,
- other factors (eg, the amount of protein in the urine, which means the kidneys are not working well).
- If chronic kidney disease is left untreated, it can lead to various complications:
- anemia,
- mineral and bone disorders,
- fluid overload,
- hypertension (high blood pressure),
- neurological changes,
- skin problems,
- growth and development problems,
- cardiovascular diseases (eg, left ventricular hypertrophy, calcium deposits in blood vessels),
- dyslipidemia (increased cholesterol and triglycerides in the blood),
- nutritional problems (eg, weight loss, weight gain, malnutrition),
- etc.
TREATMENT OPTIONS FOR END-STAGE RENAL DISEASE (ESRD)
Dialysis
- Dialysis is a treatment that replaces the elimination function of the kidneys. It cleans the blood of waste and excess by passing it through a filter, much like healthy kidneys would do. Dialysis does not replace the production function of the kidneys.
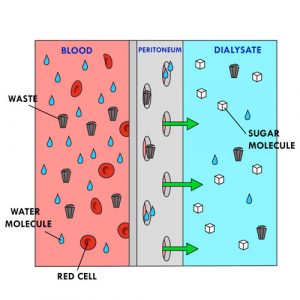
- During dialysis, blood is on one side of the filter and a special solution (dialysate) is on the other side. The waste products from the blood pass through the filter and into the dialysate. Larger particles (eg, red blood cells) remain in the blood. The cleaned blood returns to the circulation and some of the waste is removed.
- Dialysis does not cure kidney disease, but it reduces the discomfort and improves the quality and length of life.
- In addition to dialysis, the child must take medication and follow a special diet to treat possible complications of kidney disease.
- Dialysis is sometimes used temporarily in situations of acute kidney disease.
- When the kidneys stop working permanently (as in end-stage renal disease), the child must have regular dialysis treatments. Unless the child has a kidney transplant or receives supportive care (see below), dialysis must be continued for life.
Kidney transplant
- This surgical procedure allows for the transplantation of a kidney in good condition from a living or cadaveric donor. This kidney takes over and does the work that the child’s kidneys can no longer do.
- The child must take anti-rejection medication for life.
- The transplant does not cure the kidney disease, but the child can live a more normal life.
Supportive care other than dialysis (conservative/palliative care)
- This treatment consists of medication and a special diet, which slows the deterioration of kidney function and reduces symptoms.
- For some children, a kidney transplant or dialysis is not a good option. Supportive care aims to improve the quality of life while minimizing suffering.
- Even though a child is receiving dialysis treatment, the kidney disease is still present. The child must still follow a special diet and take certain medications to avoid complications.
- There are two kinds of dialysis. With the help of the healthcare team, the family chooses the type of dialysis that is best for the child based on their condition and lifestyle.
TYPES OF DIALYSIS
Hemodialysis
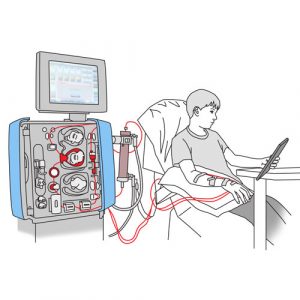
- Hemodialysis filters and cleans blood outside the body using a machine and an artificial filter called a dialyzer (or artificial kidney).
- This dialysis is made possible by placing a central venous catheter in a large vein at the base of the neck or by making an arteriovenous fistula (connecting a vein and an artery) in the arm. The machine removes blood through the catheter or fistula and passes it into the dialyzer. The dialyzer removes waste and excess water. The machine returns the cleaned blood to the circulation through the catheter or fistula.
- The blood is cleaned in this way three times a week or more frequently in young children.
- Each treatment usually takes four to five hours.
- Hemodialysis for children is done in the hospital; it can also be done at home, but less frequently.
Peritoneal Dialysis (PD)

- Peritoneal dialysis uses the peritoneum (thin membrane that lines the inside of the belly) to filter and clean the blood inside the body.
- A special solution (dialysate) is injected into the peritoneal cavity through a catheter installed in the peritoneum. The blood surrounding the peritoneum is brought into contact with the dialysate. Excess water and blood waste pass into the dialysate. The soiled dialysate (effluent) is drained out of the body through the same catheter.
- The exchange of solutions is mostly done at night with a machine (cycler) or can be done manually during the day.
- Peritoneal dialysis is usually done at home.
- Peritoneal dialysis has several advantages:
- gives autonomy and control in the child’s care,
- allows for a more flexible schedule,
- facilitates travel because it can also be done outside the home,
- requires fewer days away from school and fewer trips to the hospital,
- allows for less fluid restriction,
- allows for less dietary restriction,
- allows for better blood pressure control,
- maintains remaining kidney function longer.
- With proper monitoring and daily care, peritoneal dialysis is effective and safe at home. It allows your child to continue to grow and develop well.
How does it work?
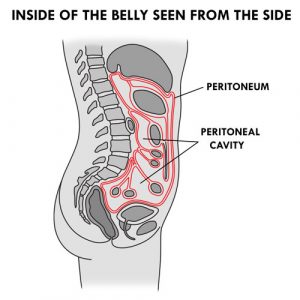
- The peritoneum is the cavity inside of the abdomen that holds internal organs (eg, stomach, intestines, liver) and helps to hold these organs in place. The lining of the peritoneum is called the peritoneal membrane. The space between the organs is called the peritoneal cavity.
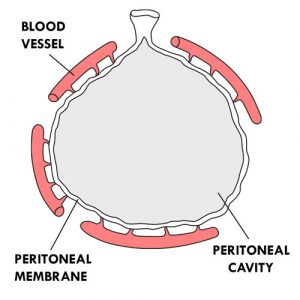
- The peritoneum can be compared to an inflatable balloon. The interior of the balloon corresponds to the peritoneal cavity and the walls of the balloon to the peritoneal membrane. The “balloon” (peritoneum) is deformed to go around the internal organs. The peritoneal membrane contains millions of tiny blood vessels.
- The peritoneal membrane has several characteristics that allow it to act as a filter:
- it is porous (filled with small microscopic holes),
- it is semi-permeable (lets water through but not large particles such as red blood cells),
- it is bi-directional (liquids can pass on both sides),
- it has a large surface area (0.5 to 2 square meters, depending on the child’s body surface).
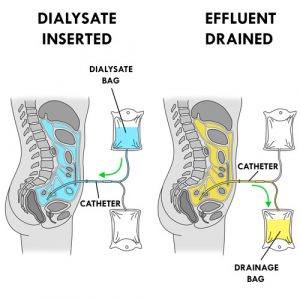
- The operation of peritoneal dialysis is simple. A special solution (dialysate or dialysis solution) is injected through a catheter into the peritoneal cavity. The blood is separated from the dialysate by the peritoneal membrane. The blood, containing waste products, excess water and mineral salts, comes into contact with the dialysate, which contains no waste products. The water and waste products pass through the peritoneal membrane from the blood to the dialysate. The dialysate absorbs the waste products and the surplus of mineral salts and water from the blood to the filtering capacity of the peritoneum. The good elements remain in the blood (eg,, red blood cells). The soiled dialysate (effluent or drainage fluid), filled with waste, is then drained through the same catheter outside the body into a drainage bag before being discarded. The effluent is yellow in color like urine.
- Peritoneal dialysis is done through exchanges. Each exchange (or cycle) consists of three phases:
1. drainage phase: exit of the soiled dialysate (effluent) from the peritoneal cavity to the outside;
2. infusion phase: entry of the new dialysate into the peritoneal cavity;
3. dwell (or contact) phase: period of time during which the dialysate remains in the peritoneal cavity and the cleaning of the blood takes place; the waste products and the surplus of water and mineral salts of the blood pass through the peritoneal membrane and go into the dialysate, which becomes progressively soiled.
- The volume of dialysate introduced during the infusion phase depends on the child’s weight or body surface area. Depending on the child’s specific needs, several exchanges must be performed to remove some of the waste products from the blood and make the child feel better. This treatment is not painful.
- The filtration of blood by the peritoneum is done thanks to two natural processes which can last from several minutes to a few hours:
- diffusion: movement of waste through a semi-permeable membrane (eg, the peritoneum). The waste passes from a medium where it is more concentrated (eg, blood) to a medium where it is less concentrated (eg, the dialysate) until there is a balance on both sides of the membrane.
- osmosis: movement of water molecules through a semi-permeable membrane (eg, the peritoneum) from a solution where there is more water (eg, blood) to a solution where there is less (eg, the dialysate), until a balance is reached. The water crosses from a less concentrated medium to a more concentrated medium.
- The dialysate is a sterile solution containing sugar (eg, glucose, dextrose), mineral salts (eg, sodium, calcium, magnesium, chlorine) and a buffer solution containing lactate, bicarbonate or lactate-bicarbonate) at an acidic (5.5) or neutral (or physiological) pH (7.4).
- It is the large sugar molecules in the dialysate that draw excess water into the bloodstream by osmosis. The concentration of sugar in the dialysate varies according to the amount of water to be removed. The higher the sugar concentration, the more water molecules in the blood are drawn into the dialysate. On the contrary, the lower the sugar concentration, the less water molecules in the blood pass through into the dialysate.
- This process is called ultrafiltration (UF). It is also referred to as the “balance” which represents the difference between the dialysate entering the abdomen and the fluid leaving it.
- At the end of a dialysis session, a positive balance refers to the dialysate retained by the child. For example, a 500 ml infusion with a 400 ml drainage corresponds to a positive balance of + 100 ml. The child retained 100 ml of the 500 ml administered. A negative balance refers to the dialysate and excess fluid removed from the child. For example, a 500 ml infusion with a 700 ml drainage corresponds to a negative balance of – 200 ml. The child has therefore eliminated 200 ml more than the amount of dialysate infused.
- The sugar concentration of the dialysate is indicated by the color of the pull ring on the bag:
- white: 0.5%
- yellow: 1.36% or 1.5%
- green: 2.27% or 2.5%
- orange: 3.86% or 4.25%
The bag with the purple pull ring contains 7.5% icodextrin which is glucose polymer.
- Each dialysate bag has:
- an injection port: allows you to add medication to the solution,
- a hanger hole: to hang the bag,
- a connector: to connect the bag to a tubing for treatment,
- a cannula (or cone) in the stem of the connector: breaking the cannula allows the solution to flow out,
- a pull ring: to protect the end of the connector; its shape facilitates its removal to connect the connector to a line (or tubing) for treatment.
- There are several types of dialysate, with varying concentrations and sizes. Here are the ones that are most often used for children at home:
SORT OF DIALYSATES
(Source: Baxter International Inc.)
Physioneal™
- Contains glucose/dextrose in concentrations of 1.36%, 2.27% or 3.86%, sodium, calcium, magnesium, chloride, lactate and bicarbonate.
- Available in 2.5 and 5 liter bags.
- Has a neutral pH (7.4).
- Has two chambers (or compartments) containing different solutions.
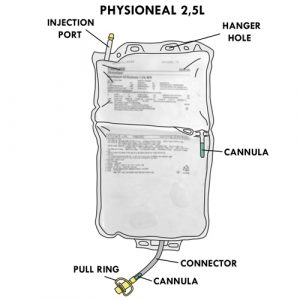
Specifics for the 2.5 liter format:
- Has a cannula between the two chambers, to be broken to mix the solutions.
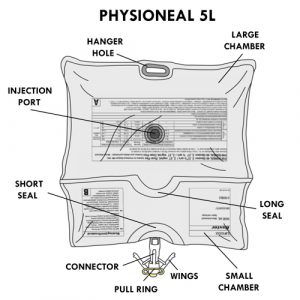
Specifics for the 5 liter format:
- Has a small and a large chamber.
- The injection port is located at the back of the large chamber.
- Has two seals:
- a long seal separates the two chambers; the opening of the long seal allows mixing of solutions.
- a short seal separates the small chamber from the connector; the opening of the short seal will allow the solution to flow into the connector.
- The connector has wings: closing the wings advances the connector cannula to puncture the bag and allow the solution to flow into the tubing for treatment.
Dianeal™
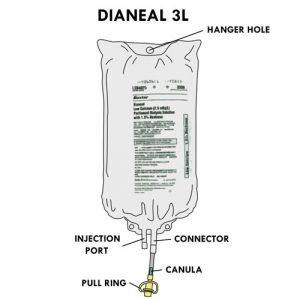 Contains glucose in concentrations of 0.5%, 1.5%, 2.5% or 4.25%, sodium, calcium, magnesium, chloride and lactate.
Contains glucose in concentrations of 0.5%, 1.5%, 2.5% or 4.25%, sodium, calcium, magnesium, chloride and lactate.- Available in 2, 3 or 5 liter bags.
- Has an acidic pH (5.5).
Extraneal™
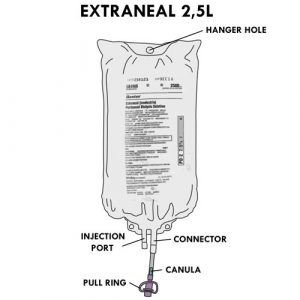
- Contains icodextrin (a molecule larger than glucose) in a concentration of 7.5% as well as sodium, calcium and magnesium, chloride and lactate.
- Available in 2.5 liter bags only.
- Has an acidic pH (5.5).
- Used once a day for a long dwell time.
- The amount of waste and water removed during a dialysis session depends on the type and concentration of the solution, the duration of the dwell phase and the filtration capacity (permeability) of the peritoneal membrane. Sometimes the healthcare team will recommend a change in the type of dialysate during the course of treatment because of certain signs of dehydration or fluid overload present in the the child (eg, rapid weight change, blood pressure too high or too low, presence or absence of swelling, etc.). Do not hesitate to discuss this with your child’s healthcare team.
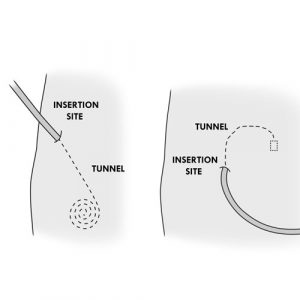
- Peritoneal dialysis requires the installation of a small flexible tube, the peritoneal catheter, to allow the dialysate to enter and exit the peritoneal cavity. This catheter is installed surgically in the abdomen, on the right or left side. Different types of catheters can be used.
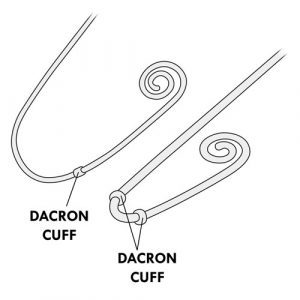
- The catheter has an external and an internal part. The catheter has one or two dacron cuffs in the internal part, allowing it to be stabilized under the skin and inside the peritoneal cavity. These cuffs are not visible from the outside.
- The catheter insertion site (or entry site or catheter site) is the skin around the catheter. The bump or line you feel under the skin a few inches from the catheter insertion site is the beginning of the inner part and is called a “tunnel”. The tunnel is the path of the catheter under the skin, from the insertion site to the peritoneal cavity.
-
- The child keeps the catheter in place as long as he or she requires peritoneal dialysis, for weeks, months or years. The catheter is connected to a titanium adapter, which in turn is connected to an extension (or transfer line). This extension is protected by a MiniCap disconnect cap between dialysis sessions. The catheter insertion site is covered with a dressing.
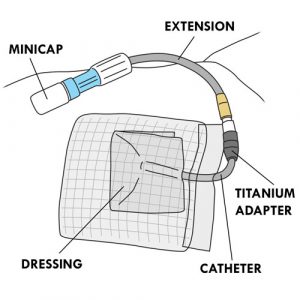
- The child keeps the catheter in place as long as he or she requires peritoneal dialysis, for weeks, months or years. The catheter is connected to a titanium adapter, which in turn is connected to an extension (or transfer line). This extension is protected by a MiniCap disconnect cap between dialysis sessions. The catheter insertion site is covered with a dressing.
- There are two methods of peritoneal dialysis. Each has its advantages and disadvantages. With your help, your healthcare team will identify the one that best suits your child’s needs.
METHODS OF PERITONEAL DIALYSIS (PD)
Automated PD (APD)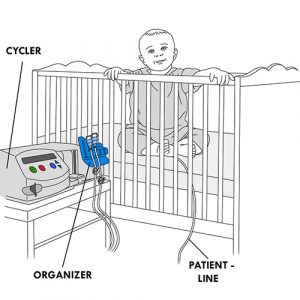
- Automated method using a device (cycler) with constant or no presence of dialysate in the peritoneal cavity.
- It consists of approximately four to ten short exchanges at night, according to a pre-established program in the cycler. Daytime exchanges may also be added, depending on the child’s needs.
- The dialysate is injected and drained from the peritoneal cavity automatically by the cycler.
- This type of peritoneal dialysis is the most frequently used at home for children.
Several types of programming are possible. The most frequently used are:
- Continuous cyclic PD (CCPD): In addition to the nighttime exchanges, a longer exchange during the day is added. The cycler is disconnected in the morning upon awakening; dialysate remains in the peritoneal cavity during the day. In the evening, at bedtime, the effluent is drained after connection to the cycler for the night.
- Intermittent PD (IPD): Drainage is performed in the morning. The peritoneal cavity remains empty during the day.
Continuous Ambulatory PD (CAPD) or Manual PD
- Manual method with constant presence of dialysate in the peritoneal cavity.
- Usually consists of four exchanges per day, at regular intervals: morning, noon, late afternoon and at bedtime. The dwell phase is longer at night.
- The dialysate enters and leaves the peritoneal cavity by gravity.
- This type of dialysis is not very common at home in children. It is mainly used in emergencies when the cycler is not working.
- The equipment required for automated peritoneal dialysis includes several accessories:
AUTOMATED PERITONEAL DIALYSIS (PD) EQUIPMENT
(Source: Baxter International Inc.)
Cycler
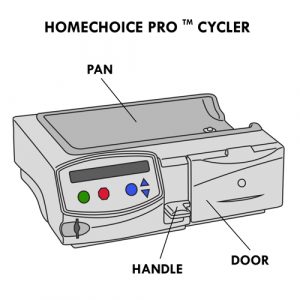
- There are different models of cyclers (eg, HomeChoice, HomeChoice Pro MC).
- Some models allow the use of a memory card to record data.
- The handle of the cycler locks/unlocks the compartment where the APD cassette is installed.
Cycler set with cassette or APD set
Contains several parts:
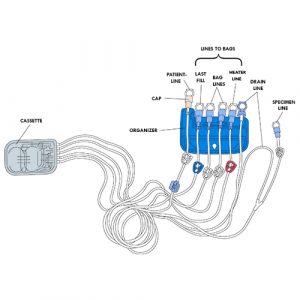 Cassette: has two separate compartments; one is used to measure the amount of dialysate infused and the other the amount of effluent drained.
Cassette: has two separate compartments; one is used to measure the amount of dialysate infused and the other the amount of effluent drained.- Organizer: allows the grouping of tubing in a specific order for use.
- Lines (or Tubings):
- specimen line: is Y-shaped with the drain line; is used to connect the specimen bag if needed; has a white clamp.
- drain line: installed at the far right of the organizer; used to connect the drain bag; does not have a clamp.
- heater line: used to connect the bag placed on the heater (empty or full bag); has a red clamp.
- bag lines (or supply lines): are used to connect the dialysate bags for the duration of the treatment, if needed; have white clamps.
- last fill line: is used to connect the last dialysate bag for daytime use if the type of solution is different from the solutions used at night; can also be used as an additional bag line if the same dialysate is used for the entire treatment; has a blue clamp.
- patient line: installed on the far left side of the organizer; connects the child with the catheter extension for treatment; has a white clamp.
(Click to see larger image)
- The end of each line is protected by a protective cap.
- The set model used for peritoneal dialysis is specific to children. However, when the volume of dialysate to be injected is ≥ 1000 ml, your healthcare team may suggest that you use the adult model.
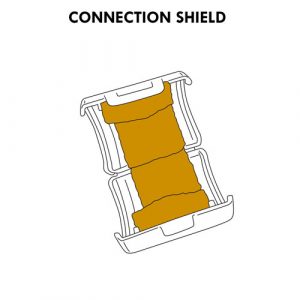
- The patient line tip is different between the two models:
- the patient line tip of the pediatric (child) set fully covers the catheter extension tip when connected;
- the patient line tip of the adult set only partially covers the end of the catheter extension when connected; some healthcare teams recommend installing a connection shield with povidone-iodine to protect the exposed portion of the extension.
5-Prong manifold set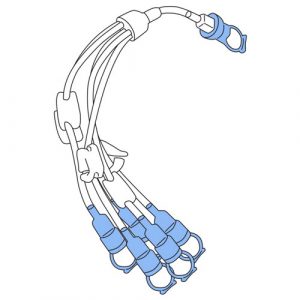
- Allows connection of additional dialysate bags if the 2 bag lines are not sufficient.
- Each line has a clamp and its end is protected by a protective cap.
Drainage bag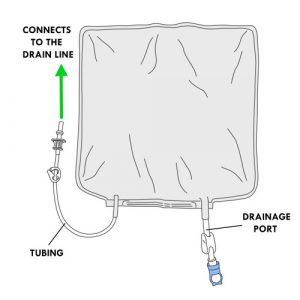
- Collects effluent.
- Has a tubing with a perforator protected by a protective cap.
- This tubing connects to the drain line of the cycler set with cassette.
- Has a drainage port to empty the effluent; its is protected by a protective cap.
Specimen bag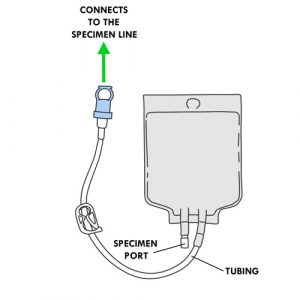
- Collects the effluent specimen.
- Has a tubing protected by a protective cap.
- This tubing connects to the specimen line of the cycler set with cassette.
- Has a specimen port for removing effluent with a syringe.
Empty bag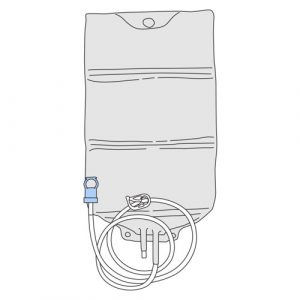
- Installed on the heater as needed.
- Is used when the child needs a mixture of dialysates with different concentrations and small volumes infused per cycle.
Dialysis clamp
- Allows you to clamp the catheter in case of emergency, disconnection or breakage of the catheter.
Depending on the recommendations of your healthcare team, can also be used to:
- secure the closure of the drainage bag tubing through which the effluent is drained;
- clamp multi-line extension and bag lines not connected to a dialysate bag during treatment.
- Refer to your healthcare team for:
- the type of dialysis solutions to use,
- the frequency of exchanges to be performed,
- the operation of the cycler, if applicable.
- Unfortunately, peritoneal dialysis cannot replace everything that healthy kidneys do. The child must therefore follow a specific diet and take vitamins and medication as recommended by the healthcare team.
Your healthcare team is available to supervise the care provided to your child, ensure the proper functioning of equipment and make recommendations to you as needed.
Refer to your healthcare team if the equipment used for your child at home is different from what is described in this section or in the methods of care.










